31
JANUARY, 2025
Casting the Future of AI-First Medicaid Systems
Imagine stepping into an elegant hotel lobby. The atmosphere is calm, welcoming, and efficient. At the center is a single concierge desk— staffed by a hospitality expert who knows every detail of the hotel and the surrounding city. This concierge can handle any request, help you with information, and arrange access to specific experiences. You feel confident, supported, and understood.
Now, imagine that same level of personalized, seamless service embedded within your state’s Medicaid system. One number. One point of contact. One intelligent system ready to serve every beneficiary, provider, and administrator with the same care and precision as that luxury concierge.
For Medicaid Recipients: Effortless Support, Personalized Care
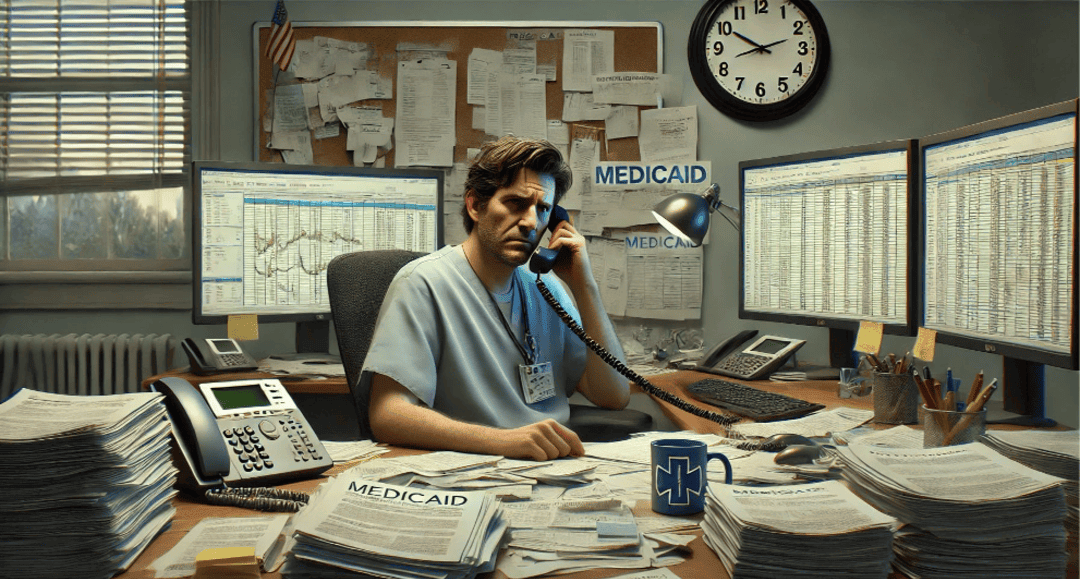
Before: Navigating Medicaid often results in frustration and, in some situations, despair — dialing multiple numbers, explaining your situation repeatedly, and getting transferred between departments and forcing people and families under stress and with precious limited time to attempt to navigate a complex system in hopes of helping themselves or their loved ones.
Future State: Now, a Medicaid recipient simply calls one number. A warm, intelligent AI voice answers and introduces themselves, greeting them by name after securely verifying their child’s identity and the mother as the listed legal guardian through advanced authentication measures, ensuring full HIPAA compliance.
“Good afternoon, Maria. How can I assist you today?”
Maria doesn’t need to know who to call. She simply says, “I need to understand if my son’s medication refill is covered. He needs a refill badly; without it, his sickness will get bad again, and I’ll miss work.”
The AI acknowledges her distress, and in seconds, the AI accesses her profile, reviews her plan, and responds with precise, helpful information.
Since her needs require human support from the provider to approve the refill, the AI seamlessly transfers Maria to the exact specialist—no holds, no repeats. It also stages the required refill request with her provider’s office for human review.
Outcome: Maria feels relieved, empowered, and respected. She was able to quickly get what she needed to keep her boy on the upswing and not risk missing any work.

For Healthcare Providers: Tailored Support for Every Role
Before: Providers spent hours navigating mazes of websites and documents and misdirected calls to a list of phone numbers based on topic, often with long hold times, confusing instructions, and disjointed online portals, documents, websites, and human support queues.
Future State: Every healthcare professional now accesses Medicaid support through the same intelligent system with integrated touchpoints – saving time, whether it’s a hospital administrator, a billing specialist, a nurse, or a physician.
- Medical Billing Staff: Calls to verify coverage or clarify claim denials are instantly directed to AI-powered billing support that retrieves relevant policy details and claims statuses.
- Hospital and Office Administrators: Need to check on provider enrollment or compliance updates? The AI system offers real-time insights, policy clarifications, and submission tracking without endless searches.
- Physicians and Nurses: Like Dr. Lee, clinicians requesting prior authorizations or needing patient eligibility checks are swiftly guided through streamlined processes or connected to the right team—with full access to necessary patient data.
- Coordinated Field Support: The AI system schedules follow-up calls or on-site visits from Medicaid field representatives when in-person support is necessary. Whether it’s resolving complex billing issues or providing compliance training, providers receive proactive, hands-on support when needed.
- Provider Enrollment Assistance: New providers navigating enrollment can call for step-by-step guidance. The AI agent answers enrollment-related questions and actively guides users through the provider portal in real-time, directing them to the correct sections of the enrollment forms while on the call.
For Medicaid Administrators: Intelligent Insights, Streamlined Operations
Before: Managing disjointed call centers, juggling data silos, responding reactively to problems and needing to expend significant resources to execute program integrity goals.
Future State: The AI-first system becomes the central nervous system of Medicaid operations. Administrators have real-time access to system analytics—identifying bottlenecks, tracking call resolution rates, and detecting trends that impact program performance.
Sarah, a Medicaid program director, receives proactive alerts about emerging trends: a spike in benefit inquiries following a policy change. The AI suggests tailored communication strategies to preempt confusion. It also flags potential compliance risks, ensuring adherence to Program Integrity goals without added administrative strain.
Outcome: Operational efficiency increases, resources are optimized, and administrators can demonstrate to federal and state oversight bodies that Medicaid is running a highly effective and compliant program.

A Seamless Ecosystem of Care
This AI-first Medicaid system is not just a technological upgrade—it’s a transformation. It offers:
- Unified Access: One number, one portal, one intelligent system.
- Personalized Interactions: Tailored responses and proactive care.
- Operational Efficiency: Reduced costs and optimized workflows.
- Empowered Users: Beneficiaries, providers, and administrators all experience clarity, support, and ease.
- Accountable Governance: Enhanced transparency and performance aligned with Program Integrity goals.
Like a luxury concierge, this system anticipates needs, simplifies complexity, and elevates every interaction—ensuring that your state’s Medicaid is not just a program but a trusted partner in health and well-being.
The Path Forward
We implement a single, unified phone line supported by a competent AI-enabled Automated Voice Response System (AVRS) to begin welcoming a more efficient future. This foundational step will streamline communication, coordinate support, and provide accurate real-time information.
From this solid starting point, we will continuously learn and expand the system’s capabilities—driving forward the mission of cost-effective and resource-efficient administration, fostering collaborative care provision, and enhancing the quality of experience for every Medicaid recipient. This evolution ensures that North Carolina Medicaid remains a beacon of innovation, care, and operational excellence.
